Prescription Medication Prior Authorization Explained

Prescription Medication Prior Authorization Explained Youtube Key takeaways: prior authorizations are required by insurance companies for some medications. this includes those that may have less expensive alternatives. the prior authorization process usually takes about 2 days. once approved, the prior authorization lasts for a defined timeframe. you may be able to speed up a prior authorization by filing. Insurance companies and pharmacy benefits managers (pbms) require prior authorization for certain prescription medications in order for them to be covered.pr.
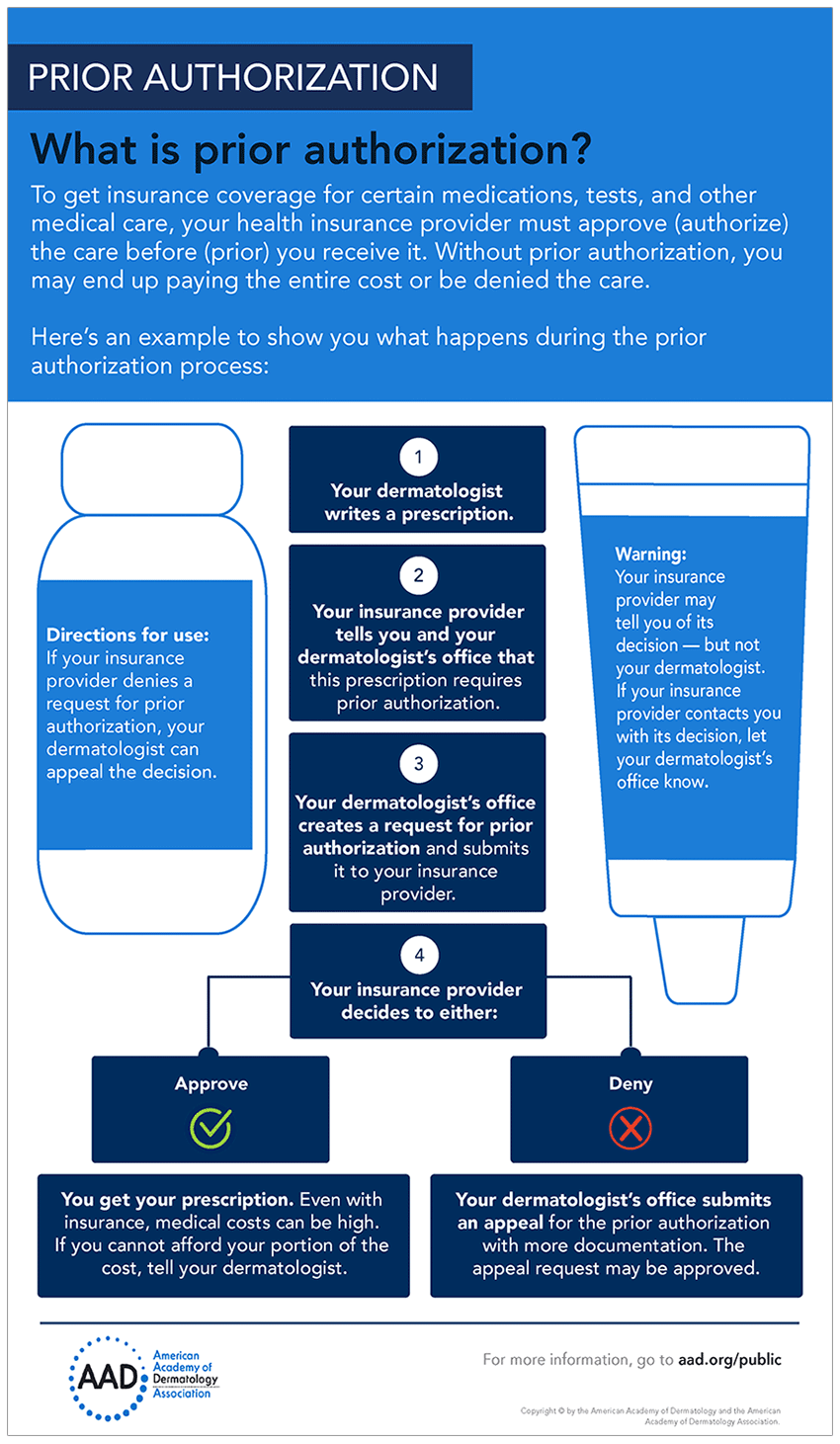
Prior Authorization Process Flow Chart The prior authorization process can be explained like this: in some cases, your doctor will recommend a treatment plan that your insurance may not cover. this is when they need to get approval from your insurance provider to know if your plan will cover it. this approval process is called prior authorization, and getting one before you get care. Insurance companies and health plans use prior authorization to make sure that a specific medical service is necessary and being provided cost effectively . your health plan uses prior authorization as a way to keep healthcare costs in check. ideally, the process should help prevent too much spending on unnecessary medical care. Before filing a prior authorization request, ensure the patient is eligible for the proposed treatment or medicine under their insurance plan. the next step is to verify the patient's insurance coverage and any treatment or medication restrictions. step 2: determine if a code or service requires prior authorization . In cases involving prescription drugs, however, the pharmacy usually notifies the doctor that prior authorization is required. after being notified, the healthcare provider initiates the process. the prior authorization process typically involves communicating with the insurance company and filling out forms that may be specific to that.
Comments are closed.