Quality Payment Program An Inside Look

Quality Payment Program 2018 Basics Youtube There are 2 ways clinicians can choose to participate in the quality payment program: the merit based incentive payment system (mips): if you’re a mips eligible clinician, you’ll be subject to a performance based payment adjustment through mips. advanced alternative payment models (apms): if you decide to take part in an advanced apm, you. Quality payment program (qpp).

Cms Awards 100m To Help Small Practices Implement Quality Payment Description. this zip file includes: the 2024 quality payment program (qpp) final rule overview fact sheet and a set of frequently asked questions (faqs). help shape the future of qpp. participate in a user feedback session. sign up now. resources. Fact sheets the quality payment program. This video provides an overview of the quality payment program (qpp). the video explains why qpp was created, lists its program objectives, and introduces qp. Quality payment program overview.
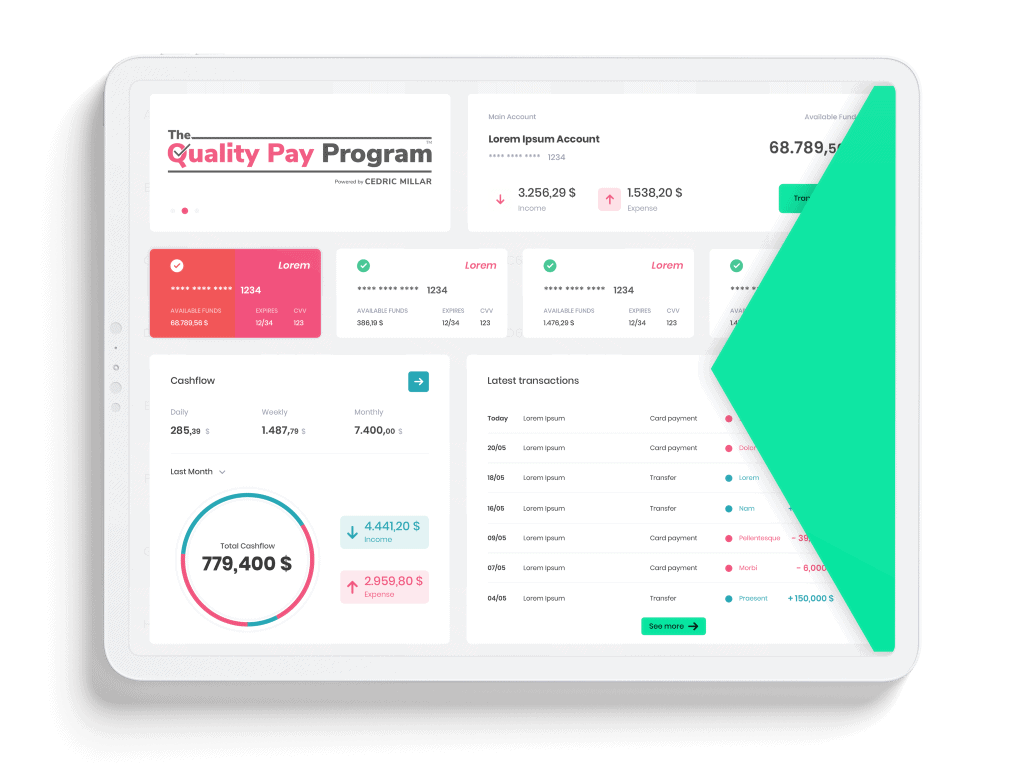
Leading Supply Chain Technology The Quality Pay Program This video provides an overview of the quality payment program (qpp). the video explains why qpp was created, lists its program objectives, and introduces qp. Quality payment program overview. The quality payment program policy will reform medicare payments for more than 600,000 clinicians across the country, and is a major step in improving care across the entire health care delivery system. you can choose how you want to participate in the quality payment program based on your practice size, specialty, location, or patient population. Meeting the thresholds for qualifying participant (qp) in an approved advanced apm exempts providers from participating in the mips and makes them eligible for a 1.88% incentive payment and higher conversion factor update to medicare payments. in 2024, the thresholds for qp are at least 75% of medicare part b payments or see at least 50% of.
Comments are closed.